Orthorexia nervosa can present as simply being health-conscious. I’ve seen how it can take over patients’ lives.

Sign up for the Slatest to get the most insightful analysis, criticism, and advice out there, delivered to your inbox daily.
Mia came to therapy for issues unrelated to food. She came because she couldn’t sleep, couldn’t turn off her brain, couldn’t stop running through her to-do list long enough to feel like a person instead of a machine. She was an accomplished executive-level professional with a demanding job and under relentless pressure to perform. She described herself as disciplined, high-functioning, healthy. From the outside, it certainly would look that way.
As Mia (not her real name) spent weeks talking about stress management with me, I noticed the outline of something else gradually took shape. She planned her meals days in advance. Her eating patterns were rigid and rule-bound. She traveled with protein powder and Ashwagandha gummies. At the time, she didn’t see any of this as problematic. When I asked how she would describe her relationship with food, she replied, “Clean. Healthy. High-protein.” Then she laughed. “Why? Do you think I have an eating disorder?”
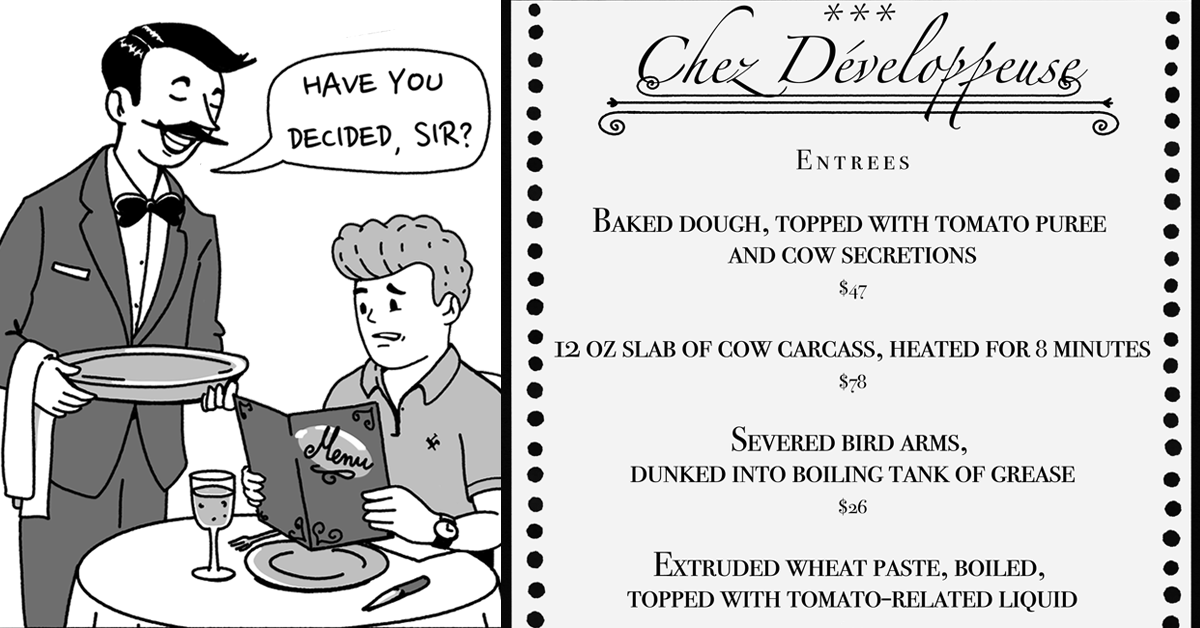
Orthorexia, a term first coined in 1997 by physician Steven Bratman, combines the Greek words for correct and appetite. It describes an obsession with healthy eating that can lead to extreme psychological distress and medical consequences. Because it often masquerades as self-control or health-consciousness, orthorexia is easy to overlook, even by people suffering from it. But under the surface, these rigid food rules can be a coping mechanism for anxiety, trauma, or a need for control.
Though not formally recognized in the DSM-5, the term orthorexia has gained traction as wellness culture has exploded. Clinicians continue to debate how best to define it, as orthorexia can share features of anorexia nervosa and obsessive-compulsive disorder. But for those affected and those who treat them, the technical debate is beside the point.
“Even in the absence of formal diagnostic criteria, we see firsthand how orthorexia can seriously disrupt someone’s life and health,” said Molly Perlman, chief medical officer of Monte Nido, a national network of eating-disorder treatment centers. “This isn’t just a wellness routine gone too far. It can result in significant medical issues, social isolation, and psychological impairment, on par with the other eating disorders we treat every day.”
People with orthorexia are not necessarily driven by a desire to lose weight or exist in a thin body. Instead, their behaviors are often motivated by deeply held values and rigid thinking around purity, self-control, and identity: They must follow portion sizes and nutrition recommendations to the letter and read all the latest news about what ingredients can cause disease. In a culture that elevates wellness to a moral ideal, these patterns often fly under the radar, even when they end up taken to an extreme.
For Mia, it started in her mid-20s, when she began experiencing migraines and gastrointestinal distress. A friend suggested she might be sensitive to gluten. In an effort to feel better, Mia began eliminating food groups: first gluten, then refined sugar, then anything not labeled organic. What began as symptom management evolved into a strict way of living.
This kind of restriction in response to medical uncertainty is a common starting point for orthorexia. It was, in fact, the very context in which Bratman first observed the pattern.
“When I invented the term, I was an alternative-medicine doctor,” Bratman explained. “Patients would come in, asking right away what foods they should cut out, like that was the answer to so many problems. It just startled me, how virtuous people felt about it, and it cultivated this incredible personal rigidity. I could see the harm it was causing.”
When conventional medicine fails to offer clear answers, especially for vague or chronic symptoms, people may turn to food as a form of self-treatment. Cutting out “bad” ingredients can feel empowering, offering a sense of control in the midst of confusion. But that control can quickly become rigid, narrowing food choices and reinforcing fear. Over time, this pattern, which is unlikely to resolve the underlying medical concerns it set out to fix, becomes associated with high levels of psychological distress and significant social impairment.
Evidence indicates that orthorexia is on the rise. Although prevalence rates are difficult to estimate in the absence of standardized diagnostic criteria, recent studies suggest that the condition may affect anywhere from under 1 percent to nearly 7 percent of the general public. Among certain groups, including athletes, nutrition students, and health professionals, the numbers are significantly higher, with some studies reporting rates of over 50 percent.
Christy Harrison, a registered dietitian and author of The Wellness Trap and the Substack Rethinking Wellness, knows this firsthand. She experienced orthorexia in her early years as a dietitian.
“I was very rigid in my food consumption, day to day,” she said. “And I was literally teaching nutrition courses at farmers markets about the benefits of all these unprocessed, locally grown foods. I didn’t think it was a problem. I thought I was just being healthy.”
Given the constant stream of content about which foods to avoid, it’s easy to see how orthorexia can flourish. These behaviors, like avoiding sugar or eating only organic produce, are often ego-syntonic, meaning that they feel correct, or virtuous, rather than problematic.
That’s part of what makes orthorexia so insidious. Unlike disordered-eating behaviors like binging or purging, which often prompt concern or intervention, orthorexic actions are likely to be overlooked or even praised.
Orthorexic patterns often extend beyond food. Mia used only organic cleaning products, avoided plastic containers, and refused to keep paper towels at home. Much of her week was spent planning meals, researching ingredients and products, and consuming wellness content focused on what to avoid. Though they started from a place of wanting to feel better, her efforts quietly crowded out joy, connection, and ease.
These behaviors were tied to a larger drive to be good, to purify, to eliminate anything “bad.” As Bratman puts it, “You lose the goal out of love for the medium. You find a path to a goal, but then you fall in love with the path and lose track of the goal.”
In other words, what begins as a pursuit of health can become a prison.
It’s important to distinguish orthorexia from general health-conscious behaviors. Bratman advocates for the term orthorexia nervosa to capture when those behaviors become disordered. “There are people who just want to eat more fruits and vegetables and get regular exercise,” he explains. “They might read labels to avoid added sugar. But reading food labels doesn’t mean you have orthorexia.”
Entering the territory of an eating disorder typically involves a significant level of psychological distress tied to one’s thoughts or behaviors. This might include persistent anxiety about eating the “right” way or noticing that food rules are consuming a disproportionate amount of time and mental energy.
Harrison encourages her clients to reflect on whether their food beliefs or behaviors are interfering with their relationships. “Is it affecting your loved ones? Are friends or family saying that this is harming their relationships with you in some way?”
Mia often skipped social gatherings that involved food, ate beforehand, or agreed only to restaurants that served locally sourced ingredients. Her world gradually became smaller. Her overall anxiety increased, and the effort to maintain control over her eating left her feeling depleted and alone. What once felt like a path to health began to erode her sense of connection and joy.
Recognizing the problem and finding effective treatment can be complicated by the sheer volume of wellness content on social media. Harrison recommends creating distance. “It tends to be more helpful for people to unfollow triggering accounts, unsubscribe from emails, block ads,” she said. Both Bratman and Harrison emphasize the importance of approaching health and nutrition media, which often present very specific ingredients as “bad” or “good,” with skepticism and a critical eye. As Bratman puts it: “All the important rules of healthy eating can be listed in a single paragraph, and they are not very exciting.” In other words, it makes sense to eat lots of vegetables, include protein with meals, and avoid excess sugar. But when nutrition becomes a full-time job, it may be time to ask what else is going on.
For many, recovery involves reintroducing foods step by step and learning to separate health from morality. It also means looking underneath the behavior to understand what the need for control was protecting them from in the first place. That might include helplessness, shame, grief, or a deeper sense of uncertainty.
“Like other eating disorders, treatment for orthorexia focuses on nutritional stabilization, reestablishing consistent eating patterns, and gradually reintroducing foods that have been labeled as ‘bad,’ ” says Perlman, the Monte Nido chief medical officer. “It’s about helping individuals reconnect with their internal cues and reducing the fear that’s come to be associated with food.”
Mia resisted loosening her food rules at first, then acknowledged that her resistance was likely part of the problem. As she began to challenge her rigid beliefs, she noticed her stress levels decreasing and her energy returning. Flexibility with food gave her more than just dietary variety; it opened up her life. What started as small exposures in the therapy office, like adding dressing to a salad or eating a packaged snack, translated into real-world moments: sharing tortilla chips at a happy hour, eating lasagna at a family meal, saying yes instead of calculating a way out. Recovery made space for spontaneity, connection, and relief.
In a world that prizes “clean eating,” orthorexia thrives, often hiding in plain sight. But as awareness grows, so does the possibility for change.
Sign up for Slate's evening newsletter.






 English (US) ·
English (US) ·